Understanding SADI-S (Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy)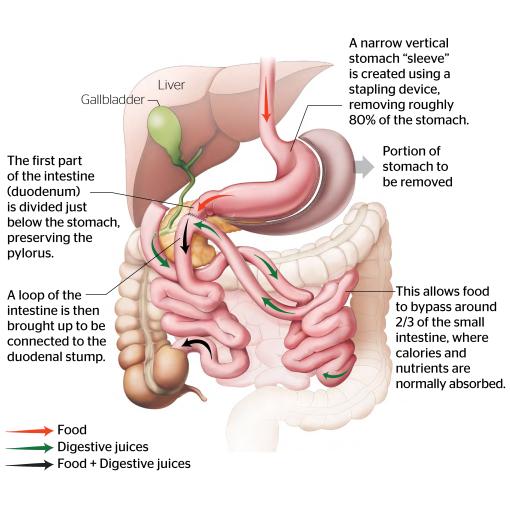
Single Anastomosis Duodenal-Ileal bypass with Sleeve Gastrectomy (SADI-S) is an advanced bariatric procedure designed to aid significant weight loss and improve obesity-related health conditions. It combines two surgical elements: a sleeve gastrectomy, which reduces the size of the stomach, and a bypass of a portion of the small intestine, which alters nutrient absorption. This dual approach promotes both restriction of food intake and malabsorption of calories, making it an effective treatment option for severe obesity.
The SADI-S has evolved from the traditional biliopancreatic diversion with duodenal switch (BPD/DS), a well-established weight loss surgery known for its powerful effects on weight reduction and metabolic improvement. While the BPD/DS involves two intestinal connections (anastomoses), the SADI-S simplifies the procedure by creating a single anastomosis between the duodenum and the ileum. This reduces operative time and potential complications without compromising the effectiveness of the surgery.
Comparison with Other Bariatric Operations
Compared to other bariatric operations, such as the Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG), SADI-S offers a higher degree of malabsorption, making it particularly suitable for patients with a high body mass index (BMI).
Compared to Roux-en-Y Gastric Bypass
Unlike the Roux-en-Y gastric bypass (RYGB), where the stomach is divided to create a small gastric pouch and the intestines are rerouted in a "Y" configuration, SADI-S preserves the pylorus, the valve at the lower end of the stomach. This preservation plays a significant role in regulating the passage of food from the stomach to the intestines, resulting in a lower incidence of dumping syndrome—a condition where undigested food rapidly enters the small intestine, causing symptoms like nausea, abdominal pain, and diarrhoea. By maintaining the natural gastric emptying process, SADI-S provides a more physiological approach to digestion.
Additionally, the single anastomosis in SADI-S connects the duodenum (the first part of the small intestine) to the ileum, rather than connecting the intestine directly to the stomach as in RYGB. This anatomical difference reduces the risk of developing marginal ulcers, a complication often seen in RYGB due to exposure of the newly created gastric pouch to stomach acid. Because of this lower ulcer risk, patients who have undergone SADI-S can safely use nonsteroidal anti-inflammatory drugs (NSAIDs), which are usually contraindicated in RYGB due to the heightened ulcer risk.
Compared to Sleeve Gastrectomy
In SADI-S, a wider bougie is used during the sleeve gastrectomy compared to a standard sleeve gastrectomy, resulting in a wider sleeve. This provides a larger stomach capacity while still limiting food intake. The addition of the intestinal bypass in SADI-S enhances weight loss and metabolic benefits, combining both restriction and malabsorption to achieve more effective long-term outcomes.
Ideal Patient Profiles
- High BMI Patients: The ideal candidate for SADI-S is a patient with a high BMI who requires significant weight loss and has been unsuccessful with less invasive interventions, such as diet, exercise, and medications.
- Metabolic Conditions: Patients with poorly controlled type 2 diabetes or other metabolic conditions may benefit significantly due to the potent hormonal changes associated with SADI-S, which can improve glycemic control and lipid profiles.
- Revision Surgery: SADI-S can address weight regain or inadequate weight loss after a previous bariatric operation, most commonly a sleeve gastrectomy. The existing sleeve can be preserved, while the intestinal bypass component adds a new dimension of malabsorption, potentially leading to better outcomes.
Contraindications to SADI-S
While SADI-S can be highly effective, it may not be suitable for everyone. It is contraindicated in:
- Patients with severe GORD
- Patients with Barrett's oesophagus
- Patients with hiatus hernia of more than 4 cm
Patients with severe gastro-oesophageal reflux disease (GORD) or Barrett's oesophagus should generally avoid SADI-S, as the procedure can exacerbate reflux symptoms. In cases where GORD is present, RYGB is usually preferred due to its beneficial effect on reducing acid exposure.
Surgical Technique
SADI-S involves a two-part procedure combining a sleeve gastrectomy with a duodeno-ileal bypass. This combination allows for both restriction of food intake and malabsorption, providing a powerful tool for weight loss and metabolic improvement.
Sleeve Gastrectomy Phase
The first step in SADI-S involves performing a sleeve gastrectomy, where approximately 70-80% of the stomach is removed, leaving behind a tubular-shaped stomach. The key difference from a standalone sleeve gastrectomy is that a wider bougie (calibration tube) is used to guide the resection, resulting in a wider sleeve. This wider sleeve maintains a larger gastric capacity while still limiting food intake, aiming to balance restriction with a reduced risk of complications such as severe nausea or reflux.
The sleeve gastrectomy phase helps reduce hunger by lowering levels of ghrelin, a hormone produced in the part of the stomach that is removed. It also prepares the anatomy for the second phase of the procedure, where nutrient absorption will be altered.
Duodeno-Ileal Bypass Phase
After the sleeve gastrectomy, the surgeon performs a single anastomosis to bypass a portion of the small intestine. The first part of the small intestine, the duodenum, is divided just beyond the pylorus, which is preserved. This preservation is crucial, as it helps regulate the emptying of stomach contents into the intestines, reducing the risk of dumping syndrome.
The divided end of the duodenum is then connected (anastomosed) to a section of the ileum, typically 250-300 cm from the end of the small intestine. This rerouting creates a shorter common channel where bile and pancreatic enzymes mix with food, leading to malabsorption of nutrients and enhancing weight loss. The exact length of the bypassed segment can be adjusted based on the patient’s BMI, metabolic conditions, and other individual factors to optimise outcomes.
Variations in Technique (e.g., Differing Limb Lengths)
The length of the bypassed intestinal segment in SADI-S can be adjusted based on the patient’s individual characteristics, with the measurement starting from the terminal ileum:
Longer Common Channel (300-350 cm): Leaving a longer segment of ileum intact, such as 300-350 cm, is typically chosen for patients who may be at higher risk of nutritional deficiencies or have a lower BMI. This approach provides a more balanced mix of restriction and malabsorption, aiming to reduce the risk of long-term nutritional issues while still achieving significant weight loss.
Shorter Common Channel (200-250 cm): Leaving a shorter segment of ileum, around 200-250 cm, may be considered for patients with a very high BMI who require more aggressive weight loss. This configuration increases malabsorption, which can enhance weight loss, but also carries a higher risk of nutritional deficiencies and requires careful postoperative monitoring.
Mechanism of Action
The Single Anastomosis Duodenal-Ileal bypass with Sleeve Gastrectomy (SADI-S) promotes weight loss and improves metabolic health through a combination of restriction, malabsorption, hormonal changes, and alterations in gut microbiota. These mechanisms work together to create a powerful effect on reducing body weight and treating obesity-related conditions such as type 2 diabetes.
1. Restriction and Malabsorption as Mechanisms of Weight Loss
SADI-S combines two primary mechanisms to achieve significant weight loss:
- Restriction: The sleeve gastrectomy portion of the procedure reduces the stomach's size, limiting the amount of food that can be consumed at one time. By creating a narrower, tubular stomach using a wider bougie, the procedure allows for some preservation of gastric capacity while still providing effective restriction. This reduction in stomach volume helps patients feel full with smaller portions, decreasing caloric intake.
- Malabsorption: The duodeno-ileal bypass alters the normal digestive process by rerouting the flow of food away from the majority of the small intestine, where most nutrient absorption occurs. By connecting the duodenum to a segment of the ileum, SADI-S shortens the length of the small intestine available for absorption. This results in fewer calories and nutrients being absorbed, contributing to further weight loss. The degree of malabsorption can be adjusted by varying the length of the common channel (the portion of the intestine where bile and pancreatic enzymes mix with food), which allows for customisation based on the patient's needs.
2. Hormonal Changes Influencing Appetite and Metabolism
Reduction in Ghrelin
Ghrelin levels decrease as the portion of the stomach that produces this hunger hormone is removed. This leads to reduced hunger and helps with appetite control.
Increased GLP-1 and PYY Levels
The changes in intestinal flow and nutrient exposure boost the secretion of hormones such as GLP-1 and PYY, which play significant roles in satiety and blood sugar regulation. These hormones slow gastric emptying, promote a feeling of fullness, and enhance the body’s insulin response, making SADI-S particularly effective for patients with type 2 diabetes.
3. Impact on Gut Microbiota
Changes in gut bacterial composition due to the anatomical changes from SADI-S favor alterations in the gut microbiota that are associated with better metabolic health. These shifts help support weight loss and improve energy metabolism.
Complications and Risks
SADI-S is associated with certain risks and complications that can be classified into early postoperative issues, long-term risks, and a comparison with other bariatric procedures. One of the most serious complications unique to SADI-S is the risk of duodenal stump blowout.
Early Postoperative Complications
Duodenal Stump Blowout
This is a specific and serious complication associated with SADI-S. It occurs when there is a leak or rupture at the closed end of the duodenum (duodenal stump) after the duodenum is divided. This can lead to severe peritonitis and sepsis, requiring urgent reoperation. Careful surgical technique and proper closure of the duodenal stump are essential to minimize this risk. It is not encountered in procedures like sleeve gastrectomy or Roux-en-Y gastric bypass (RYGB), making it a complication unique to SADI-S and other procedures involving duodenal transection.
Anastomotic Leak
Though less common than duodenal stump blowout, a leak at the anastomosis between the duodenum and ileum can occur, resulting in intra-abdominal infection. Prompt recognition and intervention are crucial to manage this potentially life-threatening complication.
Bleeding
Postoperative bleeding may arise from the staple lines in the stomach or the anastomosis site. If significant, it may require a blood transfusion or reoperation to control the bleeding.
Infection
There is a risk of wound infection, especially at the incision sites. This can typically be managed with antibiotics, but may occasionally require additional intervention.
Long-Term Risks
Nutritional Deficiencies
Due to the bypass of a substantial portion of the small intestine, SADI-S carries a significant risk of deficiencies in essential nutrients like iron, vitamin B12, calcium, and fat-soluble vitamins (A, D, E, K). Lifelong nutritional supplementation and regular follow-up are necessary to prevent these complications.
Bile Reflux
Patients may experience bile reflux, as the altered anatomy allows bile to flow back towards the stomach, causing symptoms like heartburn or gastritis. While SADI-S offers advantages over RYGB for certain patients, it may not be the best choice for those with severe gastro-oesophageal reflux disease (GORD).
Diarrhoea and Malabsorption
The bypassed intestine can lead to diarrhoea or increased stool frequency, especially if high-fat foods are consumed. The altered absorption may also result in steatorrhoea (fatty stools). Adherence to dietary recommendations and nutritional monitoring is essential.
Weight Regain
As with any bariatric procedure, some patients may experience weight regain over time. This often relates to lifestyle factors and requires continued follow-up with a bariatric care team.
Internal Hernia
The risk of internal hernia in SADI-S is lower than in Roux-en-Y gastric bypass (RYGB) due to its simpler anatomy. SADI-S creates only one mesenteric space where the bowel could potentially herniate, whereas RYGB has two. However, while the risk is lower, internal hernias can still occur, especially after significant weight loss. Symptoms like intermittent abdominal pain, nausea, or vomiting should be promptly evaluated.
How SADI-S Compares to Other Bariatric Procedures in Terms of Safety Profile
Compared to Roux-en-Y Gastric Bypass (RYGB)
SADI-S has a lower risk of marginal ulcers, as the anastomosis is to the duodenum rather than the stomach, allowing patients to safely take NSAIDs. However, the risk of duodenal stump blowout is a unique and serious consideration in SADI-S, not seen with RYGB. SADI-S has a lower risk of internal hernia compared to RYGB because it involves only one mesenteric space where the bowel can potentially pass through and twist, rather than two.
Compared to Sleeve Gastrectomy (SG)
While SG avoids the risks associated with duodenal transection, it typically offers less weight loss and metabolic improvement compared to SADI-S. The more complex nature of SADI-S increases the potential for serious complications like duodenal stump blowout, which are not present with SG.










